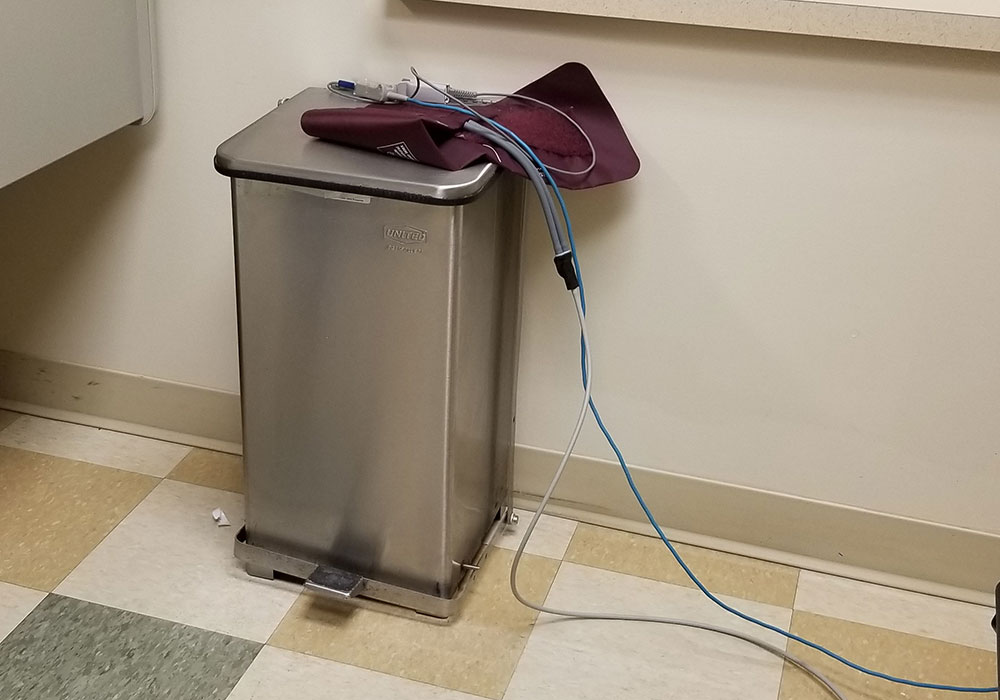
** When I initially posted this blog on why patients are afraid to speak up, a nurse friend called to say that nurses and tech staff will often have shorthand communication to indicate ‘dirty’ vs. ‘clean.’ She suggested the top of the garbage can may have been an indication the blood pressure cuff and oximeter were ‘dirty’ and in need of cleaning before the next patient. Fair enough — I was unaware of such designations and appreciative of the feedback. Are these types of communications common? Is this designation of ‘clean’ vs. ‘dirty’ protocol in your office, hospital, or urgent care center? But I admit, I am still confused. Why take something that is ‘dirty’ and expose it to an environment that is even dirtier? And what exactly are the cleaning protocols for a blood pressure cuff and oximeter?**
As a patient, have you ever been afraid to speak up, afraid to question medical professionals when something doesn’t seem quite right? Above is a picture I took during a recent visit to Urgent Care, after the nurse took my blood pressure and oxygen levels. I honestly do not know if the blood pressure cuff and oximeter used to check my vitals came from the top of the garbage can. I do know, however, it was early in the evening and this particular Urgent Care operates 24/7. There would be other patients. Why is the storage place for basic medical equipment on top of the garbage can? And, as a patient could I ask this question without fear of repercussions?
An Emphasis on Safety
Reducing infections from medical procedures is one of many goals in healthcare. Blood pressure monitoring and oxygen levels are standard procedures. Therefore, it seems careless to have frequently used medical equipment placed on top of a waste container. A garbage can is not a sterile environment. Statistics on infections within the healthcare environment show:
Healthcare-associated infections result in excess length of stay, mortality and healthcare costs. In 2002, an estimated 1.7 million healthcare-associated infections occurred in the United States, resulting in 99,000 deaths. In March 2009, the CDC released a report estimating overall annual direct medical costs of healthcare-associated infections that ranged from 28 – 45 billion.¹
Infections are an ongoing battle in healthcare. There are good reasons for protocols to reduce and/or eliminate harm. As the patient, was it safe though for me to raise this concern without offending, without repercussions to the quality of my care?
Lapses in Care Do Occur
I was visiting the Urgent Care due to an angry infection in my right eye. Red and pus-filled, my eye was unpleasant to look at and uncomfortable for me as well. The nurse who took my blood pressure put on gloves for the procedure, apologizing as she did so. She explained that the infection in my eye had a high probability of being very contagious. Fair enough. But then she turned around and placed the medical equipment on TOP of the GARBAGE CAN.
There’s a disconnect here. It’s not from a lack of knowledge or inadequate facilities. Nurses are educated, skilled medical professionals. And this particular Urgent Care Center is well funded and generally quite clean.
Why Patients Are Afraid to Speak Up
Based on my experiences, as well as others, such observations are usually not well received. About five years earlier, in the same Urgent Care center, a nurse began to insert an IV line in my arm without gloves. I needed antibiotics due to a nasty cat bite on my finger. I asked about gloves, a common step to reduce the possibility of infection. She laughed and tried to dismiss my concerns but she did put on gloves. I felt she failed to understand my concern. She did not see her action as a break in protocol, with the possibility of introducing infection. I was the one out of line for asking the question.
I’ve interviewed a number of people with serious illness for a book about the roles of advocacy and support. I met Trish at a conference focused on the intersection of Art and Medicine. Trish is a Physician Assistant (PA) with over 33 years of experience. During the conference we discovered a mutual interest on issues around physician burnout and talked frequently by phone after the conference. As a practicing PA, Trish brings both experience and perspective.
Trish’s Patient Experience
Trish was seriously ill for many years with Lyme Disease. It took nearly two years just to get a diagnosis. Her symptoms were debilitating. At one point, before the diagnosis, she was in pre-op for surgery proposed as a solution to her symptoms. In the end, the surgery was not related.
As a PA, Trish knew protocol. As a patient, she wasn’t afraid to speak up, to point out a break in procedures. But she felt the burn for speaking up:
I was in the pre-op place, and the nurse was starting an IV, and she dropped the end of the IV that was going to go in my arm on the floor and then picked it up and started to put it in my arm.
TRISH: That touched the floor.
NURSE: It’s fine, I just picked it up.
TRISH: That touched the floor.
And she, [MAKES DISGUSTED SOUND] and threw it down on the bed and marched out to the nurse’s station and another nurse came in, and she was:
NEW NURSE: Can I help you? Is there something wrong?
TRISH: The end of the IV that she’s going to put in my arm fell on the floor.
And she seemed to get upset about that. So she huffed and then she undid the tubing and she went off and got another one, then she, she made a big show of laying a sterile drape and putting things out on it and being, like, extra extra careful. But it was in a really condescending manner.
Broader Implications
As a medical professional, Trish’s concern extends beyond just this one incident. At the time of seeking medical care and treatment, patients are particularly vulnerable. How many patients don’t speak up when there are lapses in protocol because of a concern with repercussions and compromising the quality of care? Or perhaps even more worrying, there may be times when patients do not know when protocols are breached. As Trish notes:
And, and when things like this would happen to me … I was at their mercy. You’re at their mercy when you’re a patient, and you don’t want to piss them off more. Then they won’t take good care of you. And so I just sat there. But it was just one more thing that had happened to me that I was just like, shit, how many times does this happen to other people? And they don’t even have as much gumption or medical knowledge as I do to protest.
Trish
On the Same Team
As a patient, if you see a break in protocol, it is absolutely within your sphere of responsibility to speak up. Breaks in procedures meant to protect patients should be addressed. Mistakes happen and at times insufficient attention may be given, or there are distractions. Such incidents are not done with malicious intent. Yet, when they happen, patients must speak up. Your health and your life are at stake.
* Quotes in this post are from interviews conducted for my book, Navigating Illness: The Patient Experience, a work in progress. Names were changed upon an individual’s request.
¹Custodio, H.T., Steele, R.W. (2016) Hospital-Acquired Infections. Medscape. https://emedicine.medscape.com/article/967022-overview